Visceral leishmaniasis (VL) is primarily caused by L. donovani & L. infantum (synonym L. chagasi).
Visceral
leishmaniasis (VL): Clinical manifestations &
diagnosis
Visceral leishmaniasis (VL) is primarily caused by L. donovani & L. infantum (synonym L. chagasi). Leishmania can invade & replicate within host
macrophages, inducing innate & cell-mediated
immune responses. Infection usually persists after clinical cure of
the primary infection. Frequently, Leishmania
infection passes with no symptoms, which reflects the adequacy of the host immune system to manage the infection.
The ratio
of asymptomatic cases to the clinically evident infection varies according
to many factors. Most ptns with subclinical
infection are harboring viable
parasites lifelong that
may develop infection reactivation if the immune system has been compromised.
The most important clinical manifestation of VL is the syndrome known as kala-azar (Hindi for "black fever").
The incubation period is often 2-6 mo but can approach from several weeks to several
years. Onset of Sms is often insidious or subacute,
with slowly progressed malaise, pyrexia,
weight loss, as well as splenomegaly (+/- hepatomegaly)
along many months. Less often, acute febrile
illness can persist with rapid progression
of Sms.
Final Dgx requires recognition of the parasite via
either histopathology or cultured material
given by needle biopsy/ aspiration
from affected organs (e.g. bone marrow or spleen).
Aspirated samples could be inoculated into culture, while the remainder prepared in a Giemsa-stained smear. Biopsy sample could be prepared
with tissue sections and touch
preparation. Histopathologic Dgx needs to visualize the amastigotes;
culture can be performed in Novy-McNeal-Nicolle or
other parasitic media. Molecular methodology (i.e., PCR) testing can be also applied to identify
parasite in
tissues or peripheral blood.
Serology testing may include indirect fluorescent AB testing (IFA) &
ELISAs that are proved to be
efficacious. The direct agglutination testing (DAT)
needs less preparation than ELISA, so it is more suitable for developing countries.
The recombinant kinesin Ag (rK39)
is a useful Ag in ELISA assays as well as in immunochromatographic
strip formating as rapid testing.
A +ve serological
test is not
definitive proof of active VL; as these results should be interpreted in
view of the clinical as well as epidemiological
atmosphere.
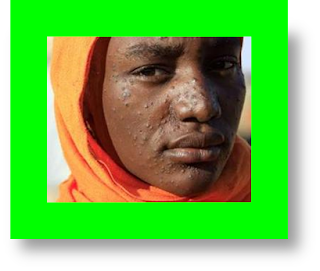
Post-kala-azar dermal Leishmania (PKDL) is a chronically observed skin rash typically
seen following clinical response to ttt for VL.
PKDL seen in almost 60 % of ptns in Eastern Africa &
in 5-15 % of VL ptns in
the Indian subcontinent. PKDL is
rarely seen in areas with L. infantum VL. It usually seen with erythematous or
hypo-pigmented macules that may be
progressed to plaques or nodules.
The Dgx can be made by assessing skin biopsy or slit skin samples by microscopy,
culture, and/or molecular techniques.
Ptns with HIV-VL
co-infection may show a lowered incidence of splenomegaly.
Among ptns with intense immunosuppression, parasitic infestation of atypical sites can be seen, including GIT, peritoneal
space, lung, pleural cavity,
& skin. HIV-VL co-infected ptns
appeared to show a relatively low AB titers but the molecular
technique have better sensitivity giving usually high levels of parasitemia in peripheral blood samples.
Histopathologic or molecular
confirmatory testing is often required for a definite Dgx.
Kidney
dysfunction: Mild renal dysfunction
seems to be present in a considerable percentage of adults & children. Most
literatures came from zones where VL
is due to L. infantum, however, one study
of pediatric VL in India reported that both parasite species can
involve the kidney.













COMMENTS